‘It was pitch black – I had to navigate a power cut in an Ebola treatment centre’

As the sun set in Uganda, Dr Tom Fletcher was engrossed in his work at the Ebola treatment centre – a heavy duty white tent pitched on the uneven ground behind Mubende hospital.
Suddenly the unit went black. A power cut forced the British infectious disease consultant and his colleague to change a struggling child’s oxygen cylinder in the dark. A fiddly process at the best of times, the pair relied on the dim glow of the digits on a pulse oximeter to finish the job and navigate their exit route.
“The light was fading and then, boom, it went pitch black,” Dr Fletcher said. “We did sort of realise, this is a little bit crazy – we’re here, surrounded by Ebola patients, and we can’t really see a thing… I would just put it under the ‘not brilliant’ definition of how you operate.”
The episode was one of the more unnerving moments during the consultant’s five week stint on the frontline of Uganda’s latest Ebola epidemic – part of an “A team” deployed by the World Health Organization to tackle particularly tricky situations.
A veteran of the devastating West Africa outbreak, which killed 11,000 people between 2014 and 2016, Dr Fletcher is no stranger to high risk scenarios. During stints working with the UK Ministry of Defence, Liverpool School of Tropical Medicine and WHO, he has also tackled diseases including Covid-19, Lassa fever, and Congo-Crimean hemorrhagic fever (CCHF).
But the 42-year-old is increasingly fed up.
“[In Uganda] I had a bad case of deja’vu,” Dr Fletcher told the Telegraph, a month after returning home to Liverpool.


“Obviously the scale of West Africa was enormous in comparison to this,” he said, referring to the 164 cases and 77 deaths reported in Uganda since mid-September. “But when you come down to it, it’s a selection of patients in a tent that you’re trying to look after – the core elements don’t change.
“What changes is your ability to look after them. Do you have better drugs? Do you have better equipment? Faster diagnostics? Do you have enough well-trained people to deliver the care that you want?
“When I reflect back to where we were at the beginning in Sierra Leone and Guinea, many of the key tools just weren’t there,” Dr Fletcher added. “And they’re still not there… it’s pretty scandalous.”
Curbing the spread
Ebola is a terrifying disease. It spreads through blood, sweat and other bodily fluids and kills around half of people who catch it.
While it is nowhere near as transmissible as Covid-19, in a highly interconnected world the threat is never far away. There have been almost weekly scares in UK hospitals among patients with Ebola-like symptoms and a travel history to East Africa this autumn.

The outbreak in Uganda was first picked up in mid-September, in a village near Mubende – a town which sits close to a major highway linking the capital Kampala to the Democratic Republic of Congo (DRC). But by this point, the virus had already gained a strong foothold.
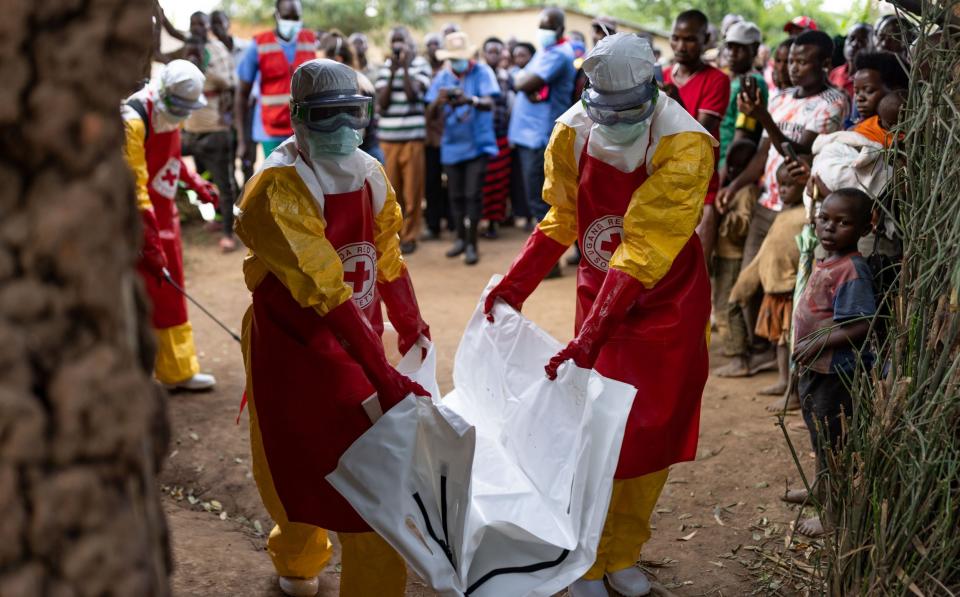
Ebola had been spreading silently for weeks, including in health clinics, and the outbreak grew quickly; contact tracing teams struggled to keep up. Tests took 24 hours to come back, while misinformation and mistrust were rife – at times cases escaped quarantine, while some families exhumed their relatives’ contagious bodies to give them religious burials.
Elements of the response were also criticised as “chaotic”; shortages of staff and supplies were “dangerous”; and a desire to avoid public health measures made unpopular during the Covid pandemic – including lockdowns – gave the virus space to spread. By mid-October, Ebola had reached Kampala, an international travel hub home to three million people.
Unlike outbreaks in West Africa and the DRC, the epidemic in Uganda was also caused by the Sudan strain – a relatively rare form of Ebola not seen since 2012, with no known vaccines or approved treatments available.
But despite huge hurdles, the national authorities and their international partners managed to get a grip on the outbreak, and Dr Fletcher praised Uganda’s “strong leadership” at grappling with the virus.
No new cases have been reported since late November and the treatment centres where Dr Fletcher worked have discharged their final patients. The experimental vaccines that arrived on Friday may never be needed – or trialled – while the two-month lockdown in Mubende was lifted on Saturday.
‘No room for error’
However, Dr Fletcher’s experience on the frontline offers lessons for future outbreaks – both of Ebola and other hemorrhagic fevers.
His criticisms are twofold: there still aren’t enough well-trained staff to respond to these pathogens; and the international community is too obsessed with vaccines – at the expense of tests, drugs and better understanding the viruses themselves.
Day-to-day, shortages of both staff and medical supplies undercut patient care and safety, Dr Fletcher said. The problem was apparent from the moment he first stepped into the treatment centre in Mubende, but was especially intense during a surge of patients around Halloween.
“We’d gone up to about 40 confirmed patients, which is a lot,” he said. “It was about eight o’clock one evening, and I was in there with a couple of the nurses and doctors. I don’t know the right phrase for it, but I was suddenly like: this is real Ebola.
“About five patients were critically ill and doing their best to die, and a lot of [the patients were delirious] or wondering. They were emitting a lot of virus – vomiting, diarrhoea, haemorrhaging – in an environment that wasn’t brilliant. You only have to make one mistake, you only need a few virus particles to infect you. So there’s no room for error. It was pretty tough.”


He added: “The doctors and nurses working there were pretty heroic and remarkable people… but they just didn’t have the environment to work in to make them successful. I guess that’s the polite way of putting it.”
As well as deficiencies of basic resources – including essential drugs and monitoring equipment – the acute shortage of hygienists throughout the outbreak undermined infection control measures in the treatment units.
These people, who aren’t necessarily healthcare workers, are the “unsung heroes” of an Ebola response, said Dr Fletcher. They’re responsible for keeping treatment units clean – including changing bed linen, scrubbing floors and ensuring hand washing facilities are available.
“There simply were not enough of them, as in, crazily low numbers… [which] unfortunately created a high risk environment for the clinical team working inside. It was a problem that we couldn’t seem to change,” Dr Fletcher said, adding that it was “remarkable” that more healthcare workers weren’t infected.
But this situation was not inevitable, Dr Fletcher said. He called for more comprehensive outbreak training among staff, as well as better preparation to ensure supply chain inefficiencies don’t delay the arrival of critical drugs and equipment.
‘I’m extremely frustrated and angry’
The consultant also said investment is needed into pandemic-fighting tools beyond vaccines. In Uganda, for instance, it took 24 hours for diagnostics to come back from laboratories to determine whether or not a patient was infectious.
“As a simple clinician looking after patients inside these tents in the back of hospitals, what I really want is the ability to diagnose patients with these diseases really quickly,” Dr Fletcher said. “And then I want to treat them really quickly, to change their outcomes.”
But this can also prove difficult. In Dr Fletcher’s view, there hasn’t been enough work to develop key tools that can be rapidly deployed and trialled should an outbreak arise – especially therapeutics.

While some progress has been made since the West Africa epidemic emerged in 2014, this has mainly been focused on the Zaire Ebola strain. The monoclonal antibodies developed are not effective against Sudan Ebolavirus. Similarly the two licensed vaccines – developed by Merck and Johnson & Johnson – target the Zaire strain.
Only six or seven courses of experimental monoclonal antibodies were available specific to the Ebola Sudan virus, partly because very few had been made to stockpile for experimental use or trials. The absence of effective drugs was “frustrating”, Dr Fletcher said, and represents a “failure” to think ahead.
This has been an issue for vaccines, too. Although the first candidates arrived just 80 days after the outbreak began, it looks like this may be too late for them to be rolled out within the community due to the sharp drop off in cases.
But Dr Fletcher is scathing about what he sees as the “short-sighted” tunnel vision on vaccines, where the majority of funding is channelled.
“I simply cannot understand [it]. This is the bit that I’m extremely frustrated and angry about – [the] short-sighted, almost unilateral focus on vaccines being the tool to get us out of epidemic or pandemic problems.
“Say for Lassa, say for CCHF, for Ebola – there are three or four major strategic goals: vaccines, diagnostics, therapeutics and better understanding the viruses themselves. But vaccines are the only thing getting significant and sustained funding,” Dr Fletcher said. “It’s awful, really.”
He added that the only way to cut the Ebola fatality rate – which currently hovers at around 40-60 per cent – is to have “better drugs and better diagnostics”. While vaccines have a critical role in containing outbreaks, treatments are “paramount” for infected individuals.
“When it comes down to it, we’re still stuck with intravenous fluids, electrolytes, antimalarials and antibiotics to treat a severe set of infections that kill half the people that get it,” Dr Fletcher said. “That has to change.”
But for now, the lack of a well-equipped toolkit for tackling Ebola means doctors working to save critically ill patients have to accept some won’t survive – a situation which never gets any easier.
“It’s pretty heartbreaking inside. When a patient's three-year-old child dies in the end next to them – it was one of the few times I’ve cried in an Ebola treatment unit,” said Dr Fletcher. “So that was pretty tough.
“But unfortunately, you’ve got to get on with it straight away and just drive on, because there’s another 25 or 30 patients … that need your care. And so that’s what you’ve got to do.”
Protect yourself and your family by learning more about Global Health Security

 Yahoo News
Yahoo News 
